The fungal kingdom encompasses a range of diverse species, including moulds, yeasts, and mushrooms. It has been estimated that there are between 2.2 and 3.8 million species of fungi. All fungi are eukaryotic organisms as their cells have a membrane-bound nucleus. Eukaryotic cells are typically much larger and more complex than prokaryotic cells, such as bacteria.
Nomenclature
Fungi are categorised using a hierarchical taxonomic system. The levels of this hierarchy (from broadest to most specific) are domain, kingdom, division, class, order, family, genus, and species. Table 1 demonstrates this classification system, using Candida albicans as an example.
Table 1. Taxonomic hierarchy of Candida albicans
| Level |
Example |
| Domain |
Eukarya |
| Kingdom |
Fungi |
| Division |
Ascomycota |
| Class |
Saccharomycetes |
| Order |
Saccharomycetales |
| Family |
Saccharomycetaceae |
| Genus |
Candida |
| Species |
albicans |
An individual species is referred to by its genus and species names. i.e. Candida albicans is a species of yeast that belongs to the genus Candida and the species albicans. The scientific convention is to capitalise all names in this hierarchy, with the exception of species name; italics are used for the genus and species.
The naming of fungal species has undergone significant changes in recent years. Nomenclature continues to evolve as new technologies improve species identification, allowing historical naming errors to be addressed. One of the most substantial naming changes occurred in 2013, where the dual naming of pleomorphic fungi was abandoned in favour of a “one fungus, one name” strategy.
Pleomorphic fungi are species that can exist in two different morphs, i.e. an anamorph (asexual) stage and a teleomorph (sexual) stage. Pichia kudriavzeveii is a good example of this issue. This species is generally considered safe and is widely distributed in the environment and used in the production of some fermented foods. However, this organism was later found to be the teleomorph of the known human pathogen Candida krusei. The currently accepted name for this species is P. kudriavzeveii.
Yeasts and moulds
Fungi that may be pathogenic to humans can occur as yeasts, moulds, or a combination of both forms.
Yeasts are microscopic single-celled fungi that typically reproduce by a process known as budding or blastogenesis. This is a type of asexual reproduction whereby a bud forms on the parent cell and grows before separating to become a new yeast cell that is genetically identical to the parent cell.
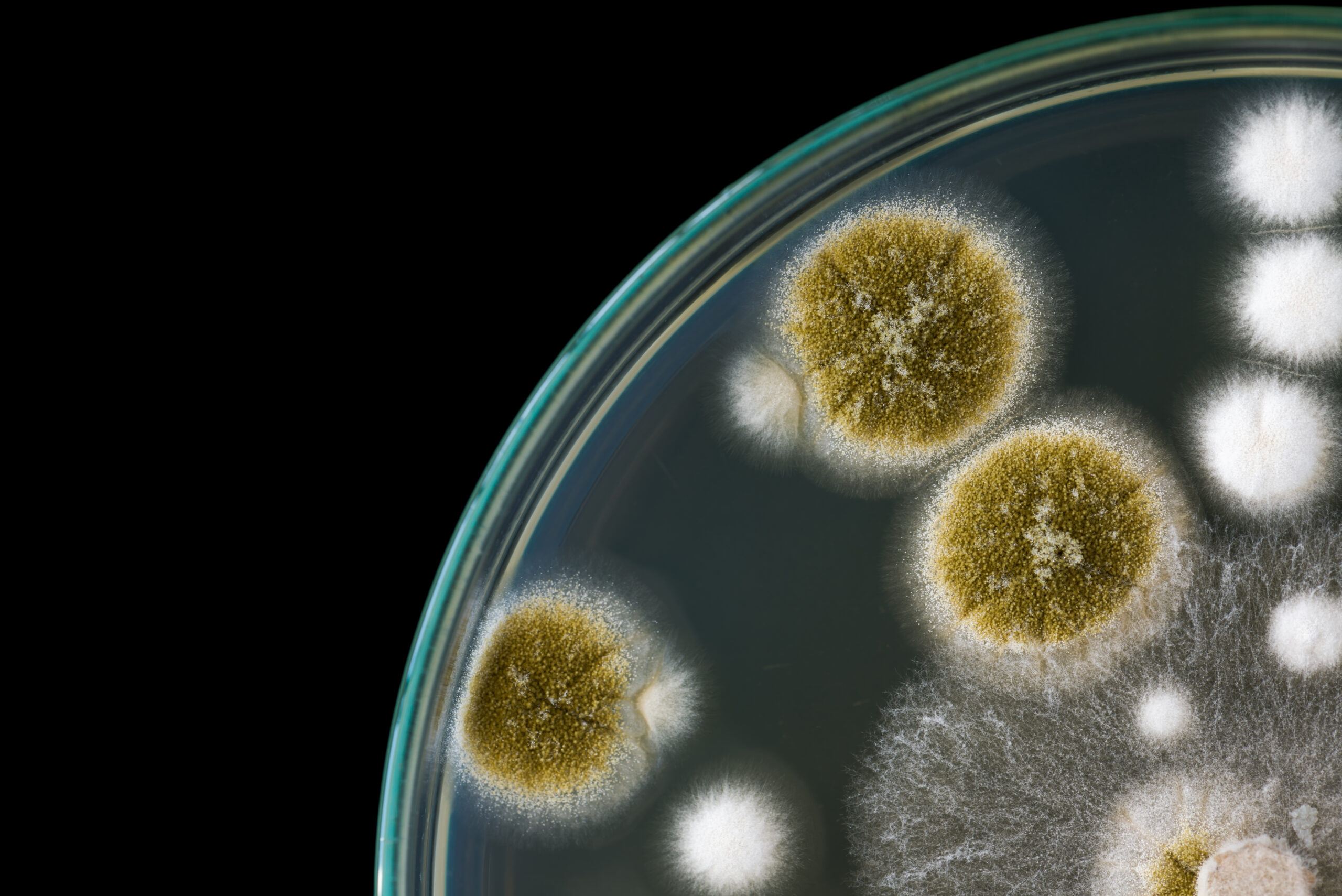
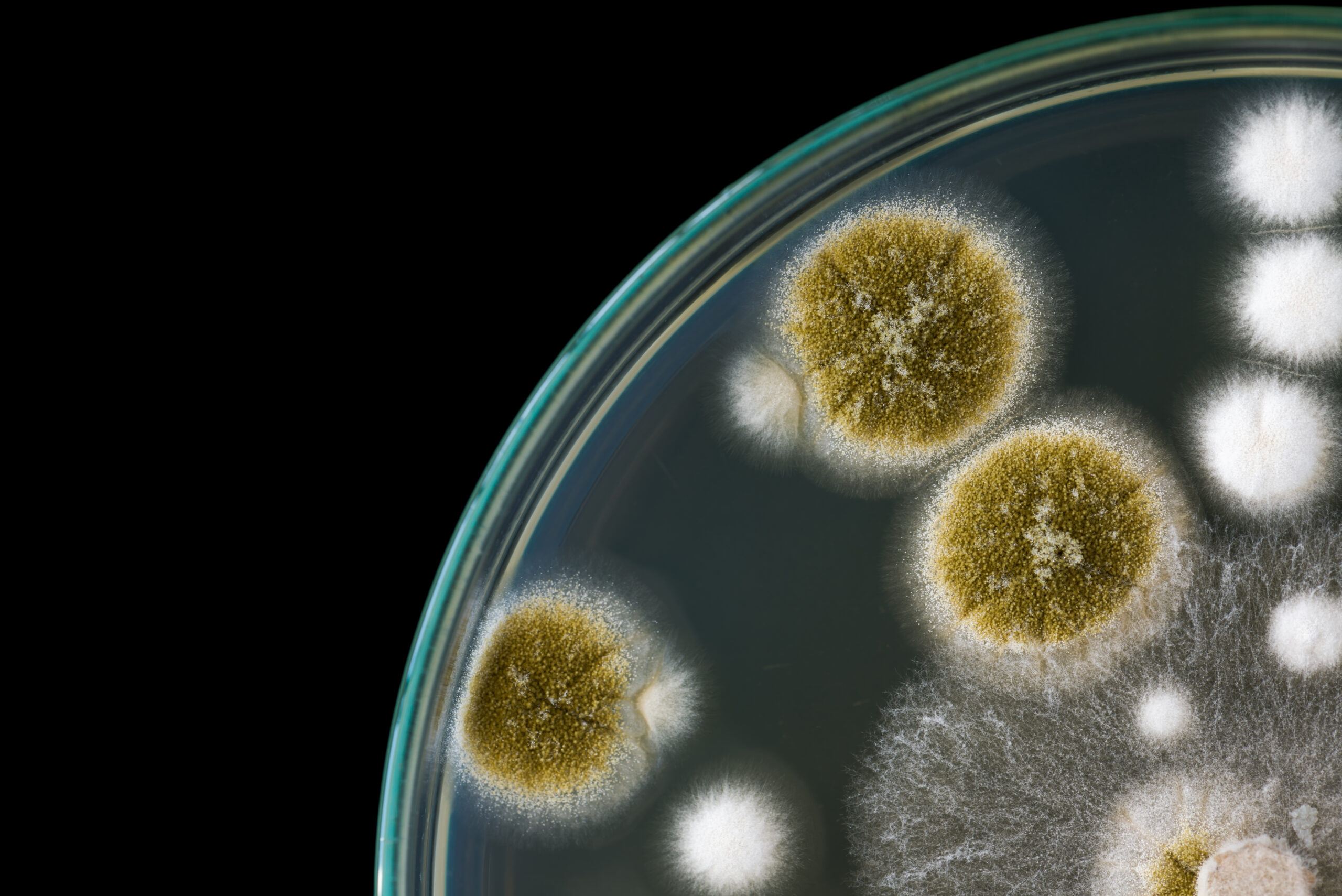
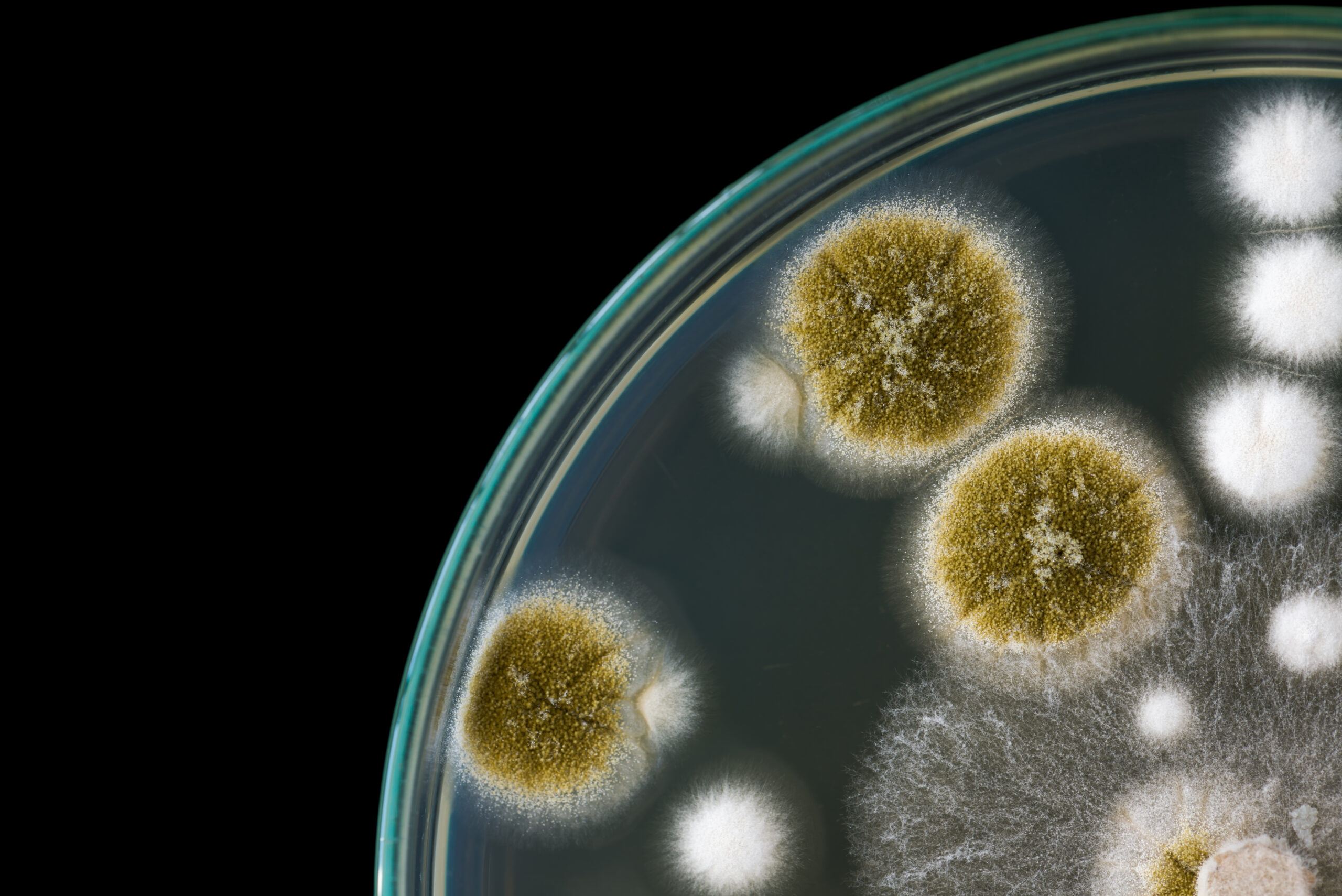
In comparison, moulds grow in multicellular filaments known as hyphae. Reproduction is primarily through the production of spores, which can be disseminated through the air or via water, animals or objects. Spores are more resistant to stressors such as high temperatures and some cleaning methods. A comparison of other features of these two forms can be seen in Table 2.
Table 2. A comparison of mould and yeast
| |
Mould |
Yeast |
| Cell |
Multicellular |
Predominantly unicellular |
| Shape |
Filamentous |
Round or oval |
| Appearance |
Fuzzy, range of possible colours |
White |
| Hyphae |
Microscopic filaments called hyphae |
Can form multicellular structures called pseudo-hyphae |
| Typical habitat |
Damp or dark conditions |
Widely dispersed in nature (e.g. on plants and fruits, soil), surface of skin and intestinal tract of warm-blooded animals. |
| Ideal growth temperature |
28℃ |
37℃ |
| Reproduction |
Spores (sexual or asexual) |
Mostly via mitosis (asexual) |
| Health risks |
Allergic reactions, respiratory problems, mycotoxins, infections. |
Infections |
| Source of energy |
Moulds produce hydrolytic enzymes that degrade biopolymers into simpler carbohydrates that can then be absorbed by the mould cell. |
Alcoholic fermentation (produces ethanol and carbon dioxide as end products of carbohydrate metabolism) |
| Examples |
Aspergillus fumigatus, Fusarium spp. |
Candida albicans, Candida auris |
Some fungi may be categorised as dimorphic. Dimorphic fungi have a yeast (or yeast-like) phase and a mould (filamentous) phase. Thermally dimorphic fungi produce a mould form between 25°C and 30°C and a yeast form at 35°C to 37°C. This allows the fungi to exist as an environmental mould and then convert into a parasitic yeast at mammalian body temperature. Dimorphic species that are considered pathogenic to humans include:
- Sporothrix schenckii (worldwide distribution with a higher prevalence in tropical and temperate regions, can cause sporotrichosis);
- Histoplasma capsulatum (found in soils with high organic content and undisturbed animal droppings, illness more likely to occur in people who are immunocompromised);
- Paracoccidioides brasiliensis (recently published Australian case of infection);
- Blastomyces dermatitidis (not typically found in Australia); and
- Coccidioides immitis (can cause Valley fever, endemic to parts of America).
Fungal infections
Many fungal species are part of the normal human microbiota. However, infections can occur that range from superficial infections to invasive infections that are life-threatening. The majority of invasive fungal infections are caused by candidiasis (around 70%); cryptococcosis and aspergillosis are also important causes.
Risk factors for developing an opportunistic fungal infection include:
- Long-term immunosuppressive therapy;
- Acquired immunodeficiency syndrome (AIDS);
- Diabetes;
- Significant burns;
- Neoplastic disease; and
- Chronic respiratory disease.
The World Health Organization (WHO) has compiled a list of priority fungal pathogens. This is a catalogue of 19 fungal species deemed the greatest threat to human health, as shown in Table 3.
Table 3. WHO fungal priority pathogens
| Pathogens |
Type |
Comment |
|
Critical group
|
| Cryptococcus neoformans |
Yeast |
Opportunistic; spread via inhalation. Cerebral cryptococcosis is life-threatening. |
| Candida auris |
Yeast |
Intrinsically resistant to most antifungals. Can cause life-threatening invasive candidiasis. |
| Aspergillus fumigatus |
Mould |
Spread via inhalation; emerging resistance to azoles |
| Candida albicans |
Yeast |
Mucosal infections or life-threatening invasive candidiasis. Low rates of antifungal resistance. |
|
High priority group
|
| Nakaseomyces glabrata (Candida glabrata) |
Yeast |
Commensal; increasingly common cause of invasive candidiasis |
| Histoplasma spp. |
Dimorphic |
Spread via inhalation; histoplasmosis more likely in immunocompromised hosts |
| Eumycetoma causative agents |
Various genera |
Deep tissue infection caused by fungi in soil and water that enter the body through breaks in the skin. |
| Mucorales |
Mould |
Fungal group causing mucormycosis, particularly in immunocompromised hosts, poorly controlled diabetes and skin and soft tissue injuries. |
| Fusarium spp. |
Mould |
Invasive fusariosis is life-threatening; innate resistance to many antifungals. |
| Candida tropicalis |
Yeast |
Commensal; can cause life-threatening invasive infection. |
| Candida parapsilosis |
Yeast |
Commensal; can cause life-threatening invasive infection. Concern in neonatal ICUs. |
|
Medium priority group
|
| Scedosporium spp. |
Moulds |
Opportunistic; can cause life-threatening invasive scedosporiosis. |
| Lomentospora prolificans |
Mould |
Opportunistic; can cause invasive lomentosporiosis in immunocompromised patients. |
| Coccidioides spp. |
Dimorphic |
Found in the Americas; can cause life-threatening invasive coccidioidomycosis. |
| Pichia kudriavzeveii (Candida krusei) |
Yeast |
Opportunistic; mucosal infections or invasive candidiasis. |
| Cryptococcus gattii |
Yeast |
Spread via inhalation; global distribution; invasive disease is life-threatening. |
| Talaromyces marneffei |
Dimorphic |
Spread via inhalation; endemic to parts of Asia; invasive talaromycosis is life-threatening |
| Pneumocystis jirovecii |
Yeast-like |
Previously known as P. carinii; global distribution; can cause life-threatening pneumonia, particularly in immunocompromised. Drug prophylaxis highly effective. |
| Paracoccidioides spp. |
Dimorphic |
Endemic to Central and South America; inhalation or penetration of skin by spores; paracoccidioidomycosis is life-threatening. |
Fungal contamination
Fungal contamination in indoor spaces can take the form of:
- Microbial volatile organic compounds (MVOCs) – fungi (and bacteria) can release a range of volatile compounds, including alcohols, ketones, aldehydes, and sulfur and nitrogen compounds. These compounds can cause local irritation of the upper respiratory tract, nose, throat, eyes, and skin;
- Mycotoxins – toxic substances produced by fungi. The most toxic mycotoxins include aflatoxins, ochratoxin A, zearalenone, trichotecenes, and fumonisins. These metabolites may be produced by various moulds, particularly Aspergillus and Fusarium Toxicity may be acute (e.g. skin irritation, diarrhoea, hepatotoxicity, nephrotoxicity) or chronic (e.g. cancer, impaired immune responses, congenital abnormalities); and
- Fungal spores and fragments of mycelia – may cause allergic reactions. Inhalation of fungal spores can cause disease, particularly in immunocompromised people.
As fungi are ubiquitous, they can pose a risk in healthcare settings. Risk factors for the proliferation of fungi within these areas include poor ventilation, dampness, and surfaces that are porous or damaged. Fungi can be introduced to a space through the air and also by personnel. Healthy adults carry a significant load of fungi, particularly on the toes and heel. However, exposed areas such as the head, neck and eyebrows may also harbour high levels. Fungi can also be introduced into a manufacturing space or drug room via packaging. Cardboard packaging is a particular concern as it can serve as a food source for cellulolytic fungi. Examples of cellulolytic fungi are Aspergillus, Chaetomium, Trichoderma, Penicillium, and Alternaria.
Fungal contamination of pharmaceutical products can lead to product spoilage. Depending on the species, ingredients in the formulation may be utilised by fungi as a source of energy. Fungi can use substances ranging from simple sugars through to complex aromatic molecules. The resulting chemical modification within the pharmaceutical product may lead to reduced therapeutic effect, reduced palatability, or pH changes that promote bacterial proliferation. For example, Aspergillus and Penicillium spp. can produce proteinases and peptidases that break down compounds in pharmaceuticals such as gelatine.
Fungal contamination also poses a risk of infection. The extent of this risk is dependent upon several factors, including:
- The type of organisms present;
- The number of organisms present;
- Route of administration for the contaminated product; and
- Patient factors.
Risk assessment
The response to fungal contamination of a pharmaceutical will depend upon whether the product is intended to be sterile or non-sterile. Any contamination of a sterile product is unacceptable. However, a risk assessment may be undertaken for non-sterile products to determine the potential for patient harm. This would include consideration of the species identified, the number of organisms present, and the type of pharmaceutical product in question.
Case studies:
Fungal contamination has led to product recalls in Australia. For example, in 2016, the Therapeutic Goods Administration (TGA) initiated a recall of one batch of acetazolamide tablets. This was due to the identification of Penicillium and Aspergillus in the bottles.
However, one of the most serious cases of fungal contamination occurred in the United States in 2012. A preservative-free methylprednisolone acetate injection was contaminated with various fungal species, primarily the mould Exserohilum rostratum. Of the more than 13,000 people potentially exposed to this contaminated product, 753 people developed infections related to the contamination and 64 deaths were recorded. Infections included fungal meningitis, localised spinal or paraspinal infections, and infections in peripheral joint spaces. This incident was later traced back to several sterility assurance failures. The significant morbidity and mortality associated with this incident highlights the importance of contamination control.
Contamination control
Areas used for pharmaceutical manufacturing or dose manipulations must be cleaned appropriately to control microbial growth. Cleaning should be regular and in accordance with a documented and validated procedure.
Decontamination processes may be divided into the following categories:
- Cleaning – physically removes dirt and grime that may harbour microbes and inactivate disinfectants;
- Sanitisers – used on surfaces to reduce the number of microorganisms, but they do not necessarily eliminate microorganisms;
- Disinfectants – used on hard surfaces to destroy or irreversibly inactivate fungi, viruses, and bacteria. These agents are not necessarily effective against spores;
- Sporicidal agents – destroy fungal and bacterial spores;
- Sterilisation – a process that destroys all microbial forms, including resistant forms such as fungi and bacterial spores; and
- Antiseptics – considered separately as they are used on living tissue to inhibit or destroy microorganisms.
Disinfectants:
Alcohol-based disinfectants, such as ethyl alcohol and isopropyl alcohol, are commonly used to disinfect surfaces. They are effective against fungi as well as bacteria and viruses. However, they are typically not effective against spores.
Isopropyl alcohol is often used in concentrations of 60-90%, with 70% being most common. The water content is important as it enhances penetration into the cell wall and acts as a catalyst in denaturing the proteins of cell membranes. The addition of water also slows evaporation of the alcohol, increasing its contact time with the surface. Once the concentration of isopropyl alcohol drops below 50%, its effectiveness as a disinfectant significantly falls. On the other hand, concentrations exceeding 90% lead to almost immediate coagulation of surface or cell wall proteins. This creates a protective layer around the microbe that prevents the alcohol from entering the cell, thereby reducing its effectiveness.
Alcohol-based cleaning products may be described as “denatured”. This denotes the inclusion of an additive that makes the product unpalatable and unfit for consumption. Other products may be labelled as “sterile alcohol”. This is a certification that the alcohol meets guideline requirements reflecting the highest standards of purity (i.e. filtered, gamma-irradiated, packaged within a cleanroom environment, etc.). Sterile alcohol is commonly used in cleanrooms, e.g. to wipe down working surfaces.
There are some disadvantages of alcohol-based disinfectants. Firstly, as they are not sporicidal and cannot penetrate protein-rich material, they are generally not appropriate for sterilising medical and surgical materials. Also, they are flammable, and their vapours can be irritating.
Sporicides
Fungal spores are more resistant to decontamination efforts than vegetative cells. However, bacterial spores are considered the most difficult to control. Many disinfectants are considered sporostatic, but not actively sporicidal against all spores. Examples include phenols, cresols, chlorhexidine, and quaternary ammonium compounds.
Sporocidal agents include glutaraldehyde, sodium hypochlorite, iodine/iodophors, hydrogen peroxide, and peracetic acid. Many of these agents can be corrosive to hard surfaces and may also present a health hazard to staff that come into contact with them. Therefore, decontamination programs may use sporicidal agents less frequently than other complementary processes.
For a decontamination process to be effective, it must achieve complete distribution and penetration of the treated area. It is also important that the product has sufficient contact time and is used at the specified concentration and environmental conditions for optimal efficacy.