Antimicrobial resistance (AMR) continues to pose a serious threat to human health, as well as the health of animals and the environment. This week is World AMR Awareness Week, a global campaign run by the World Health Organization (WHO) to increase awareness and understanding of AMR.
The theme for this year’s campaign is “Preventing antimicrobial resistance together”. Tackling AMR must be a collaborative effort across sectors and around the world. While the healthcare sector is an important driver of antibiotic use, the quantity of antibiotics used in agriculture is significant. In the US, over 70% (by weight) of the antibiotics defined as medically important for humans are sold for use in animals.
As the prevalence of AMR increases, the availability of effective antimicrobial therapies becomes more limited. In 2019, it was estimated that 1.27 million deaths were directly attributable to bacterial AMR. Future predictions suggest that the annual death toll may eclipse cancer unless decisive action is taken.
Antimicrobial stewardship (AMS) is recognised as an important component of healthcare and is included in the National Safety and Quality Health Service (NSQHS) Standards. However, many AMS programs tend to focus on antibiotics, with antifungals often not receiving the same attention.
Antifungal stewardship shares many similarities with antibiotic stewardship. They both aim to optimise antimicrobial use, improve patient outcomes, reduce adverse sequelae, ensure the cost-effectiveness of therapy, and preserve the efficacy of currently available antimicrobials. However, there are additional issues that are unique to antifungal stewardship. Invasive fungal infections (IFI) tend to affect more complex patient populations, have high mortality rates, and the therapies are often associated with greater toxicity and higher costs.
The Australian Commission on Safety and Quality in Health Care has just released the 2023 Antimicrobial Use and Resistance in Australia (AURA) report. One of the key findings is that the use of systemic antifungals in Australian hospitals has increased annually since reporting began in 2017. Increasing use of antifungals is associated with a higher risk of resistance, especially with the azole class of antifungals.
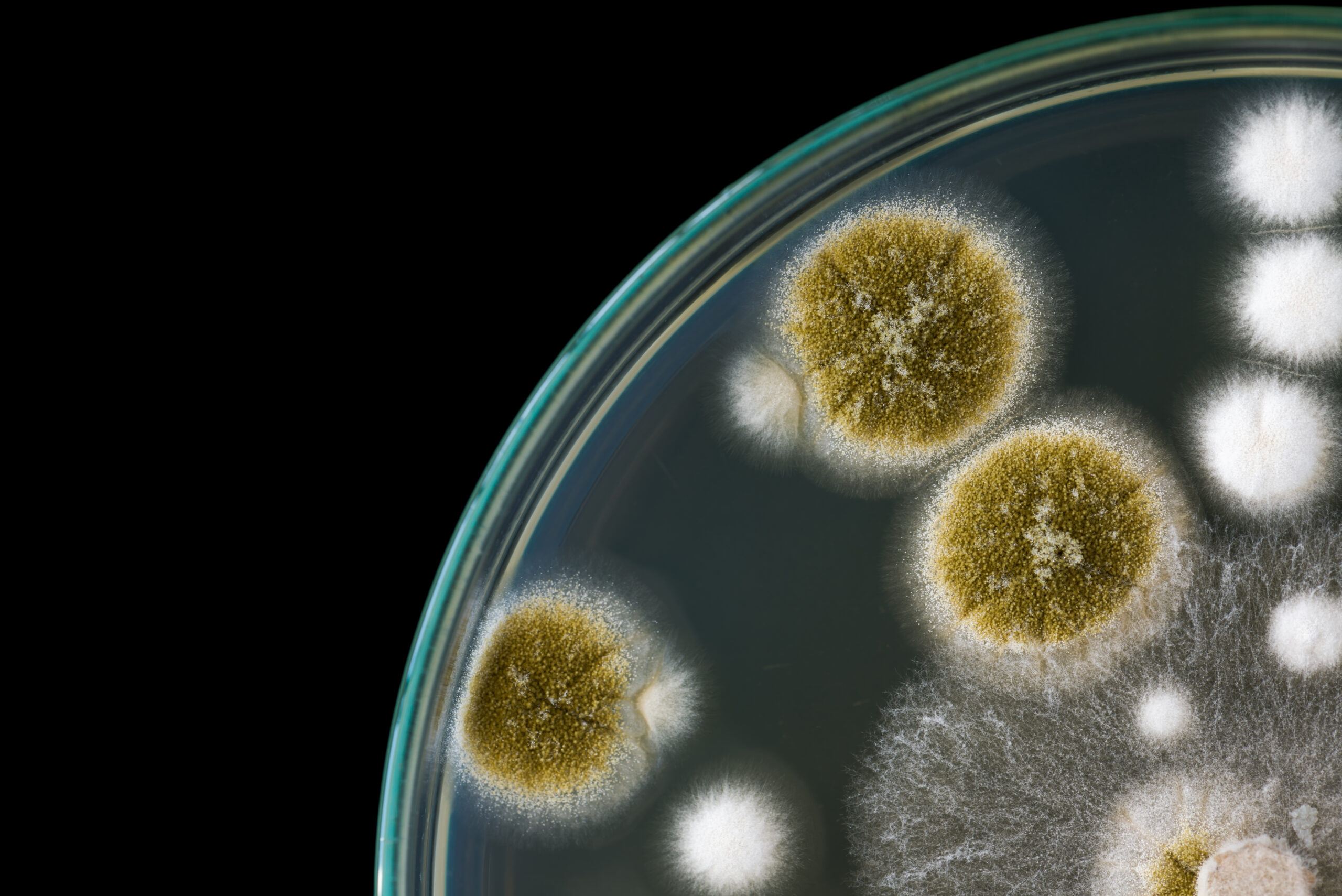
One of the focus areas highlighted in the 2023 AURA report is antifungal drug susceptibility for common Candida species and Aspergillus fumigatus complex. These species are responsible for the majority of IFIs, so emerging AMR among these species will have significant clinical implications. While antifungal resistance among these species remains uncommon, the following findings were made:
- Small numbers of Candida group isolates, particularly Nakaseomyces (Candida) glabratus, were resistant to anidulafungin and micafungin;
- Four N. glabratus isolates that were echinocandin-resistant or had intermediate susceptibility were also resistant to azoles;
- Azole resistance among Candida tropicalis and N. glabratus may be emergent (around 8%);
- Voriconazole resistance among fumigatus complex was uncommon (<5%), which supports the use of this agent as first-line therapy for invasive aspergillosis pending the results of susceptibility testing.
Antifungal resistance
Resistance to antifungals can be intrinsic. For example, Aspergillus species and many other moulds are intrinsically resistant to fluconazole. Pathogenic fungi can also acquire resistance due to selection pressure exerted by antifungal drugs. The mechanism of this acquired resistance varies depending on the antifungal agent in question.
Azoles are some of the most commonly used antifungal agents. Their primary mechanism of action is thought to be inhibition of the cytochrome P450-dependent enzyme, lanosterol 14-alpha-demethylase. This enzyme plays a vital role in the production of ergosterol, an essential component of fungal cell walls. The disruption of ergosterol synthesis by azoles causes an increase in the permeability of the fungal cell wall, resulting in cell lysis and death.
Resistance to azoles is typically acquired due to:
- Increased efflux from the fungal cell (particularly for Candida species);
- Point mutations and promotor insertions in the CYP51A gene resulting in modification of the pathway for sterol biosynthesis (for fumigatus); and
- Overexpression of the drug target and efflux pumps (e.g. Cryptococcus neoformans).
In the case of echinocandins (e.g. anidulafungin, caspofungin, micafungin), mutations of the FKS1 gene are associated with resistance in Candida and Fusarium species. In the case of polyenes (e.g. nystatin and amphotericin B), resistance is caused by loss-of-function mutations in genes coding for ergosterol biosynthesis. This is particularly evident in Aspergillus and Candida species.
Antifungal stewardship
Khanina et al. (2020) conducted a study to develop an international expert consensus on a core set of metrics for antifungal stewardship.
Days of therapy and length of therapy were agreed metrics of consumption. These metrics were considered to be of high clinical relevance as they are not impacted by individualised drug dosing and can be utilised in both adult and paediatric settings. However, feasibility was considered to be low for these metrics as they require access to patient-level data, which can be labour-intensive.
In terms of quality metrics, there was high agreement for the performance and timeliness of fungal diagnostics and follow-up for suspected invasive mould and candida infections. The effectiveness of antifungal prophylaxis is important and can be measured by rates of IFI breakthrough. Respondents considered IFI-related mortality an ideal metric for measuring the impact of antifungals at a patient level. However, this metric was considered to have low feasibility. This is due to the complex characteristics of this patient group that necessitate a detailed case review to determine the cause of death. All-cause mortality was suggested as an alternative clinical outcome. Many of the usual clinical outcomes, such as length of stay and readmission, were also rated low for importance as multiple factors are likely to influence these metrics in such a complex patient group.
The findings of this study helped inform the development of the Antifungal National Antimicrobial Prescribing Survey (AF-NAPS). The AF-NAPS is now available for use in all Australian hospitals and can be accessed via the National Centre for Antimicrobial Stewardship website. It is used to assess guideline compliance and the overall appropriateness of antifungal therapies. Assessing appropriateness using the AF-NAPS is slightly different from other NAPS audits as guidelines are not available for all indications or may not be sufficient in all clinical scenarios. A rating of appropriate can be further broken down into optimal or adequate, and a rating of inappropriate is further classified as suboptimal or inadequate. Therapies may also be rated as ‘not assessable’ if there is a lack of documentation or the patient is too complex to categorise.
Future therapies
In comparison to antibiotics, there are few antifungal classes available. Therefore, emerging resistance to these agents poses a significant threat to human health. While new antifungal therapies are needed to address this issue, few novel antifungals have been developed in the past decade.
One newer method that has been investigated involves the use of nanoparticle formulations that attempt to improve the pharmacokinetic or pharmacodynamic properties of existing antifungals. Another potential strategy for immunocompromised patients is the use of monoclonal antibodies to provide passive immunisation.
There are also some novel antifungals in phase II/III clinical trials. Rezafungin was recently compared to caspofungin in a randomised double-blind, double-dummy phase III trial. Rezafungin is a next-generation echinocandin with a broad spectrum of activity. It is currently being developed for the treatment of candidaemia and invasive candidiasis and for prophylaxis against invasive fungal disease caused by Candida, Aspergillus, and Pneumocystis species. One of the key potential benefits of rezafungin is its long half-life (around 133 hours), which allows an extended dosing interval. Results of this trial demonstrate that once-weekly rezafungin is non-inferior to daily caspofungin for the treatment of candidaemia and invasive candidiasis.
References:
- Antimicrobial Resistance Collaborators. Global burden of bacterial antimicrobial resistance in 2019: a systematic analysis. Lancet 2022; 399(10325): 629-655.
- Australian Commission on Safety and Quality in Health Care. Antimicrobial Stewardship in Australian Health Care. Sydney: ACSQHC; 2023.
- Australian Commission on Safety and Quality in Health Care. AURA 2023: fifth Australian report on antimicrobial use and resistance in human health. Sydney: ACSQHC; 2023.
- Khanina A, Douglas AP, Yeoh DK, So M, Abbotsford J, Spelman T, et al. Validation of the antifungal national antimicrobial prescribing survey (AF-NAPS) quality assessment tool. J Antimicrob Chemother. 2023; 78(6), 1367-77.
- Khanina A, Urbancic KF, Haeusler GM, Kong DC, Douglas AP, Tio SY, et al. Establishing essential metrics for antifungal stewardship in hospitals: the results of an international Delphi survey. J Antimicrob Chemother. 2021; 76(1), 253-62.
- O’Neill J. Tackling Drug-Resistant Infections Globally: Final Report and Recommendations. Government of the United Kingdom; 2016.
- Singh N. Antifungal stewardship – monitoring, metrics and the AF-NAPS. Antifungal Stewardship Workshop; 2023.
- Thompson GR, Soriano A, Cornely OA, Kullberg BJ, Kollef M, Vazquez J, et al. Rezafungin versus caspofungin for treatment of candidaemia and invasive candidiasis (ReSTORE): a multicentre, double-blind, double-dummy, randomised phase 3 trial. Lancet 2023; 401(10370): 49-59.
Subscribe Knowledge Centre Updates
Enter your details to receive Knowledge Centre updates
