The Therapeutic Goods Administration (TGA) is updating product information documents for direct acting oral anticoagulants (DOACs) to advise of the increased risk of recurrent thrombotic events in patients with antiphospholipid syndrome. Antiphospholipid syndrome is an autoimmune disorder in which patients develop antibodies to phospholipid-bound proteins. Patients with this condition are at an increased risk of thrombosis and standard treatment involves the use of anticoagulants.
Anticoagulants include heparin, warfarin, and DOACs. The three DOACs available in Australia are apixaban, dabigatran etexilate, and rivaroxaban. This new warning is based on results from the Trial on Rivaroxaban in AntiPhospholipid Syndrome (TRAPS) study conducted in patients with antiphospholipid syndrome who have a history of thrombosis and a high risk of recurrent events. This study demonstrates an increased risk of thrombotic events with rivaroxaban compared to warfarin. Thromboembolic events occurred in 21% of patients in the rivaroxaban group compared to 0% for patients in the warfarin group. Major bleeding events were reported in 7% of patients in the rivaroxaban and 3% in the warfarin group. While the study only investigated rivaroxaban, other DOACs may be associated with a similar risk.
The TGA advises that DOACs are not recommended for patients with antiphospholipid syndrome, particularly those who are considered high-risk. If these patients are currently receiving a DOAC, it may be appropriate to consider changing to an alternative anticoagulant.


Painful conditions of the mouth are uncomfortable and can significantly impair oral intake of fluid and nutrition. Mucositis is often cited as the most debilitating side effect of cancer chemotherapy and radiotherapy. Options recommended by eviQ for the symptomatic management of oral mucositis and stomatitis include systemic analgesics, topical anti-inflammatories, topical steroids, and local anaesthetic mouthwashes.
When it comes to local anaesthetic mouthwashes, there are few proprietary products available. Xylocaine® Viscous, containing 2% lidocaine, is one option. This product is formulated as a thick solution to increase adherence to the oral mucosa. Absorption from the gastrointestinal tract is relatively high, although systemic lidocaine exposure is usually low due to extensive first-pass metabolism. Caution is advised in patients with hepatic impairment as the half-life may be increased up to three-fold. While true allergic reactions to local anaesthetics are rare, Xylocaine® Viscous is contraindicated in patients with a known history of hypersensitivity to lidocaine or any other amide-type local anaesthetic.
Cocaine may be considered for patients who are allergic to amide local anaesthetics. Cocaine belongs to the ester family of local anaesthetics and does not display cross-reactivity with amides. No cocaine products are currently registered with the Therapeutic Goods Administration (TGA). However, cocaine mouthwash is produced by a TGA-licensed manufacturer and is now available in 0.5% (200mL) and 1% (100mL) strengths.
Cocaine is primarily metabolised in the plasma and tissue fluids. Its anaesthetic effect is similar to other local anaesthetics, although it does possess some unique characteristics. It is a vasoconstrictor across all dosing levels and induces platelet activation and thrombus formation. These effects may be useful to prolong the duration of effect, minimise systemic absorption, reduce swelling, and improve haemostasis in patients with mucosal bleeding.
There is a risk of systemic toxicity if used in patients with traumatised mucosa or if the recommended dose is exceeded. The estimated LD50 (lethal dose that is fatal in 50% of cases) for cocaine is 500mg for adults following oral administration. This equates to 50mL of the 1.0% solution. It is, therefore, crucial to stress the importance of adhering to dosing recommendations and to expectorate the solution following use. Caution is advised in patients with hypertension, cardiovascular disease, thyroid disease, severe hepatic impairment, or a history of drug abuse.

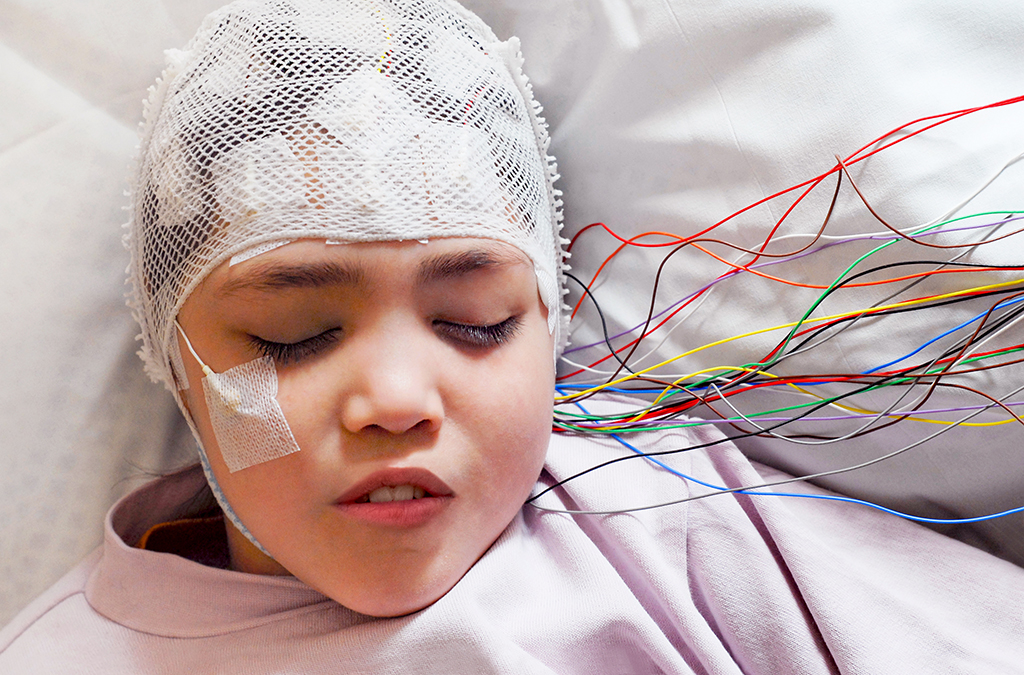
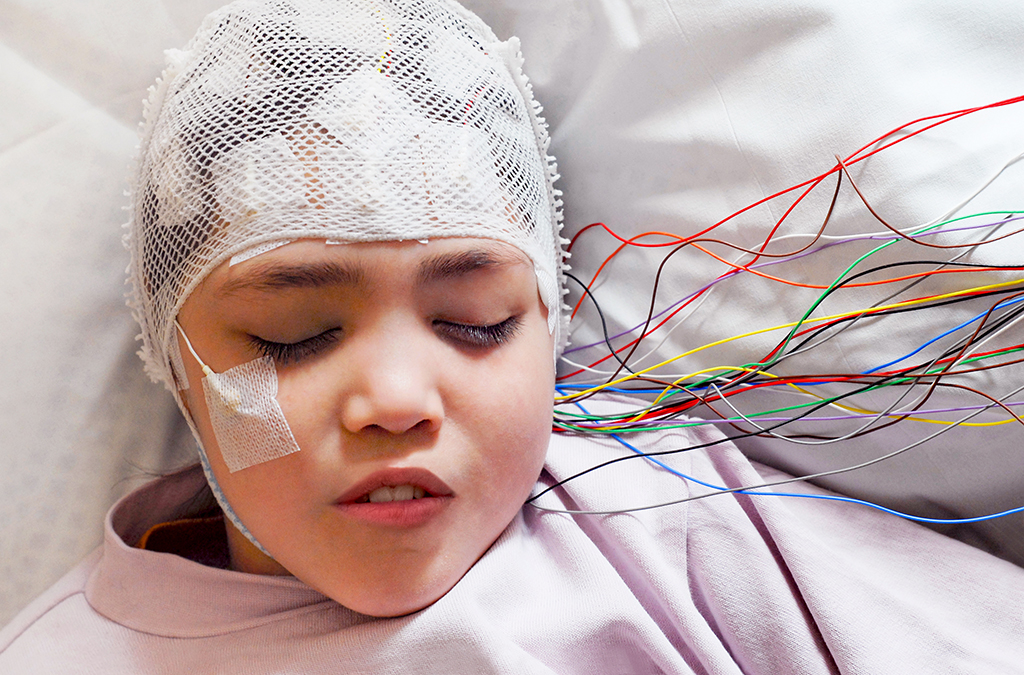
Rufinamide is a new adjunctive therapy in the treatment of seizures associated with Lennox-Gastaut syndrome (LGS). LGS is a severe form of epilepsy that presents with multiple types of seizures and is often refractory to treatment. A double-blind, randomised, placebo-controlled trial conducted in patients with LGS demonstrated a 42.5% reduction in tonic-atonic seizures in the rufinamide-treated group compared to a 1.4% increase in the placebo group. A number of other clinical trials demonstrate favourable efficacy in reducing the frequency and severity of various seizure types.
The most commonly reported adverse effects include headache, dizziness, fatigue, and somnolence. Some clinical studies have reported status epilepticus occurring in rufinamide-treated patients but not in the placebo groups. While status epilepticus is reasonably common in a population with refractory epilepsy, rufinamide therapy should be reviewed if patients experience new or increasing frequency of seizures.
Rufinamide is not metabolised by cytochrome (CYP) P450 enzymes and does not inhibit their activity to any significant extent. It is a weak inducer of CYP3A4 and may reduce the plasma concentrations of CYP3A4 substrates. Significant increases in plasma rufinamide levels can occur when valproate is initiated while rufinamide levels may be reduced by phenytoin, phenobarbital, and primidone. The absorption of rufinamide is significantly affected by food. Bioavailability and peak plasma concentrations rise by 34% and 56% respectively when administered with meals. It is advised that doses are taken with food.


Telotristat is a new medication for the treatment of carcinoid syndrome diarrhoea. Carcinoid syndrome is a condition that develops in around 10% of people with a carcinoid tumour. Carcinoid tumours develop from enterochromaffin cells, the most common type of neuroendocrine cell in the gastrointestinal tract. Tumours derived from these cells can produce large amounts of vasoactive substances, including serotonin and histamine. This may contribute to symptoms of carcinoid syndrome such as severe diarrhoea, bronchoconstriction, flushing, and abdominal cramps.
Telotristat inhibits peripheral tryptophan hydroxylase, an enzyme involved in the biosynthesis of serotonin. Consequently, serotonin levels decrease and symptoms of carcinoid syndrome are alleviated. Telotristat is designed not to cross the blood-brain barrier, and studies demonstrate no significant change in brain serotonin levels at the recommended dose. However, patients should be advised to report any symptoms of depression or altered mood to their doctor.
Telotristat is an oral medication that should be taken with food. It is indicated for use in combination with a somatostatin analogue such as octreotide or lanreotide. Short-acting octreotide causes a significant reduction in systemic exposure to telotristat and its active metabolite and should be administered at least 30 minutes after a telotristat dose.


In addition to the discontinuation of pembrolizumab 50mg vials, Merck Sharp & Dohme have advised of some upcoming changes to the Pharmaceutical Benefits Scheme (PBS) listing for the 100mg/4mL vials. These changes affect the dosing of pembrolizumab in the treatment of unresectable Stage III or Stage IV malignant melanoma.
From 1st August 2019, the PBS dosing criteria for this indication will be:
- Initial treatment – up to six doses administered every three weeks with each maximum dose fixed at 200mg; and
- Continuing treatment – maximum dose administered every three weeks fixed at 200mg.
These dosing criteria will replace the current maximum dose of 2mg/kg (up to 240mg). Pembrolizumab was first registered in Australia for the treatment of melanoma. Clinical studies used to support the initial application used weight-based doses of 2mg/kg and 10mg/kg. Later studies demonstrated equal efficacy of the higher and lower weight-based doses, leading to the introduction of a fixed 200mg dose for other indications.
The product information should be referred to for further dosing information and the PBS website for current PBS criteria. The PBS listing for the 50mg presentation of pembrolizumab will be deleted on 1st September 2019.


As discussed in Drugline Volume 354, pembrolizumab is available on the Pharmaceutical Benefits Scheme (PBS) for the first-line treatment of metastatic non-small cell lung cancer.
In the original KEYNOTE-024 trial, the median duration follow up was 11.2 months and pembrolizumab was associated with a significantly longer progression-free survival (10.3 versus 6.0 months) and overall survival at six months (80.2% versus 72.4%) compared to platinum-based chemotherapy.
An updated analysis of KEYNOTE-024 with a median follow up duration of 25.2 months demonstrated pembrolizumab to have a significantly improved overall survival (30 months vs 14.2 months) and a median duration of response not reached.
The 24-month overall survival rate was 51.5% in the pembrolizumab group vs 34.5% in the chemotherapy group.
The incidence of treatment-related adverse effects remains consistent as the interim data, pembrolizumab at 76.6% and chemotherapy at 90%. However, immune-mediated adverse effects including hypo- and hyperthyroidism, pneumonitis, skin toxicity and infusion reactions were markedly higher, with pembrolizumab at 33.8% and chemotherapy at 5.3%.


Palbociclib has recently listed on the Pharmaceutical Benefits Scheme (PBS) for the treatment of locally advanced or metastatic breast cancer. Palbociclib is a selective inhibitor of cyclin-dependent kinases (CDKs) 4 and 6. Cyclins and their complex interactions with associated kinases are important drivers of the mammalian cell cycle. Dysregulation of these processes frequently occurs in breast cancer, leading to uncontrolled cellular proliferation.
The double-blind, phase 3 PALOMA-2 study investigated the efficacy of palbociclib with letrozole compared to placebo plus letrozole. The progression-free survival (PFS) was 24.8 months in the palbociclib-letrozole group compared to 14.5 months in the placebo-letrozole group. Follow-up is ongoing to allow assessment of overall survival. The rate of Grade 3-4 adverse events was higher in the palbociclib-letrozole group, with 9.7% of patients permanently discontinuing treatment (compared to 5.9% in the placebo-letrozole group). The most common Grade 3 and 4 events reported in the palbociclib-letrozole group were neutropenia and leukopenia at 66.4% and 24.7% respectively, compared to 1.4% and 0% for the placebo-letrozole group.
Palbociclib is the second cyclin-dependent kinase (CDK) inhibitor to be listed for breast cancer following the approval of ribociclib in July 2018. The PBS conditions for palbociclib are similar to those of ribociclib in that the condition must be hormone receptor (HR)-positive and human epidermal growth factor receptor 2 (HER2)-negative and treatment must be in combination with anastrozole or letrozole. Studies suggest that palbociclib has similar efficacy to ribociclib in terms of PFS delay, overall response rate, and time to deterioration in quality of life. Their spectrum of adverse effects is also similar, although palbociclib does not appear to prolong the QTc interval.


Fiasp® is now available on the Pharmaceutical Benefits Scheme (PBS) for the treatment of diabetes mellitus. Fiasp® is a novel formulation of insulin aspart containing the excipients nicotinamide (vitamin B3) and arginine hydrochloride.
Human insulin molecules naturally self-associate to form hexamers that are too large to readily cross capillary membranes. The rate-limiting step for absorption and onset of action following subcutaneous injection is, therefore, the conversion of these hexamers into smaller units. Nicotinamide increases the rate of dissociation of insulin hexamers into dimers and monomers, resulting in faster absorption. Arginine is an amino acid that has been added to stabilise the formulation.
As nicotinamide and arginine hydrochloride are considered excipients, the generic name for Fiasp® is simply insulin aspart. It is important to note that this formulation is not interchangeable with NovoRapid®. In comparison to NovoRapid®, Fiasp® has an onset of action that is around five minutes faster and a glucose-lowering effect that is 74% greater during the first 30 minutes. Clinical trials demonstrate that this results in improved postprandial blood glucose control without increasing the overall risk of hypoglycaemia. The total and maximum glucose-lowering effect of Fiasp® is similar to that of NovoRapid®.
To avoid confusion, the Australian Commission on Safety and Quality in Healthcare recommend all insulin orders specify the full brand name of the product to be administered.


The European Medicines Agency (EMA) has announced prescribing restrictions of alemtuzumab for multiple sclerosis (MS) while a safety review is undertaken. This action is in response to new reports of serious cardiovascular and immune-mediated adverse events including heart attack, stroke, cervicocephalic arterial dissection, neutropenia, and autoimmune hepatitis.
Alemtuzumab is a monoclonal antibody active against the CD52 cell surface antigen. This protein is present on T and B lymphocytes at high levels and to a lesser extent on natural killer cells, monocytes, and macrophages. Alemtuzumab is thought to improve relapsing forms of MS through the depletion and repopulation of lymphocytes. A higher strength of alemtuzumab (MabCampath®) is also registered in Australia for the treatment of B-cell chronic lymphocytic leukaemia.
The Therapeutic Goods Administration (TGA) has not announced any action at this stage. Actions recommended by international governing bodies such as the EMA and the US Food and Drug Administration (FDA) for patients with MS include:
- Consider ceasing therapy in patients who develop signs of the abovementioned adverse events;
- Advise patients to seek immediate medical attention if they experience any symptoms of these adverse events;
- Monitor vital signs before and during alemtuzumab infusions;
- Perform liver function tests before and during therapy;
- Promptly evaluate patients who develop signs of pathological immune activation; and
- Consider other treatment options for new patients.
These serious adverse events are thought to be rare. A total of four strokes and no heart attacks have been reported to the TGA in association with both alemtuzumab formulations since the drug was first approved in Australia in 2006.


Safinamide has recently been added to the Pharmaceutical Benefits Scheme (PBS). It is indicated for the treatment of fluctuating idiopathic Parkinson’s disease as an adjunct to a levodopa-decarboxylase inhibitor combination.
Safinamide is a highly selective and reversible inhibitor of monoamine oxidase B (MAO-B). It works to increase extracellular levels of dopamine in the striatum; a region of the brain responsible for voluntary movement. Safinamide also inhibits the release of glutamate which may have additive benefits for the management of motor complications. Clinical trials demonstrate that safinamide increases daily on time without troublesome dyskinesia by up to 0.55 hours compared to placebo.
The selectivity of safinamide for MAO-B is more than 1,000 times greater than its selectivity for MAO-A. Therefore, dietary tyramine restrictions are not required. However, other medications that inhibit MAO activity must not be used with safinamide. Caution should be exercised when serotonergic agents are used concomitantly; pethidine use is contraindicated. Safinamide may also transiently inhibit the multi-drug transporter known as breast cancer resistance protein (BCRP). At least five hours should be allowed between safinamide doses and BCRP substrates such as pravastatin, ciprofloxacin, methotrexate, topotecan, and diclofenac.
The most common treatment-emergent adverse events reported in clinical trials are dyskinesia, falls, nausea, and insomnia. Retinal degeneration was observed in some animal studies. Although this effect was not reported in human trials, safinamide should be avoided in patients at higher risk of potential retinal effects. Contraindications include albino patients, retinal degeneration, uveitis, inherited retinopathy, and severe progressive diabetic retinopathy.