
Hand-foot syndrome is a side-effect which can occur with treatment with some cytotoxic drugs (e.g. capecitabine, fluorouracil, liposomal doxorubicin and cytarabine) as well as multikinase inhibitors (e.g. pazopanib, sorafenib and sunitinib). Hand-foot syndrome is also known as palmar-plantar erythrodysesthesia (PPE).
Although this side effect is not life-threatening, it can interfere with a patient’s ability to carry out normal activities. Hand-foot syndrome appears to be dose-dependent.
Pathophysiology:
In chemotherapy treatment, small amounts of drug leak out of capillaries in the soles of the foot and palms of the hands. Mechanical stress on the skin, including pressure, friction and heat increases the amount of the drug in the capillaries and increases the amount of drug leakage. This drug leakage results in redness, tenderness, and possibly peeling of the palms and soles. The redness looks like sunburn and affected areas can become dry and peel, with numbness or tingling developing.
Onset/Duration:
HFS can develop within days or weeks after starting treatment. Usually, it develops after six weeks of the treatment and mostly resolves within two weeks of stopping anticancer treatment.
Symptoms of hand-foot syndrome:
Symptoms of mild or moderate hand-foot syndrome can include:
- Redness similar to a sunburn;
- Swelling;
- A sensation of tingling or burning;
- Tenderness or sensitivity to touch;
- Tightness of the skin; and
- Thick calluses and blisters on the palms of your hands and soles of your feet.
Grading:
| Mild | Moderate | Severe | |
| Hand-foot syndrome (HFS) Grading: | Grade 1 | Grade 2 | Grade 3 |
| Minimal skin changes or dermatitis (e.g. erythema, oedema, or hyperkeratosis) without pain | Skin changes (e.g. peeling, blisters, fissures, bleeding, oedema, or hyperkeratosis) with pain; limiting instrumental ADL* | Severe skin changes (e.g. peeling, blisters, bleeding, fissures, oedema, or hyperkeratosis) with pain; limiting self-care ADL* |
*ADL: Activity of daily living
Prevention and management of HFS:
The following advice may be useful for patients undergoing therapy with agents likely to cause hand-foot syndrome:
- Having a pedicure to reduce calluses before beginning anticancer treatment;
- Apply moisturiser or emollient to avoid drying of skin;
- Protect the skin against sun exposure using a broad-spectrum sunscreen;
- Wear loose-fitting clothing and comfortable shoes with cushioned soles; avoid walking barefoot;
- Limit the use of hot water on the hands and feet when washing dishes or bathing;
- Avoid rubbing the skin after bathing; gently pat skin dry with a towel;
- Avoid using vinyl or rubber gloves. Wear lightweight dishwashing gloves as heavy gloves hold heat against the skin. Avoid washing dishes by hand if possible;
- Avoid activities that cause friction or rubbing on the hands or feet such as jogging, aerobics, power walking, jumping, or long walks;
- Avoid using household items or tools that require pressing your hand against a hard surface, e.g. screwdrivers, wrenches or knives;
- Apply cold to the tender area for relief of pain or soreness. Using a pack of frozen vegetables (15 minutes on and 15 minutes off), a hydrogel dressing, or soaking hands or feet in cold water can be helpful;
- Taking vitamin B6 may help to prevent or treat hand-foot syndrome. Patients should be advised to check with their doctor before taking any supplements; and
- Elevate hands or feet to reduce swelling.
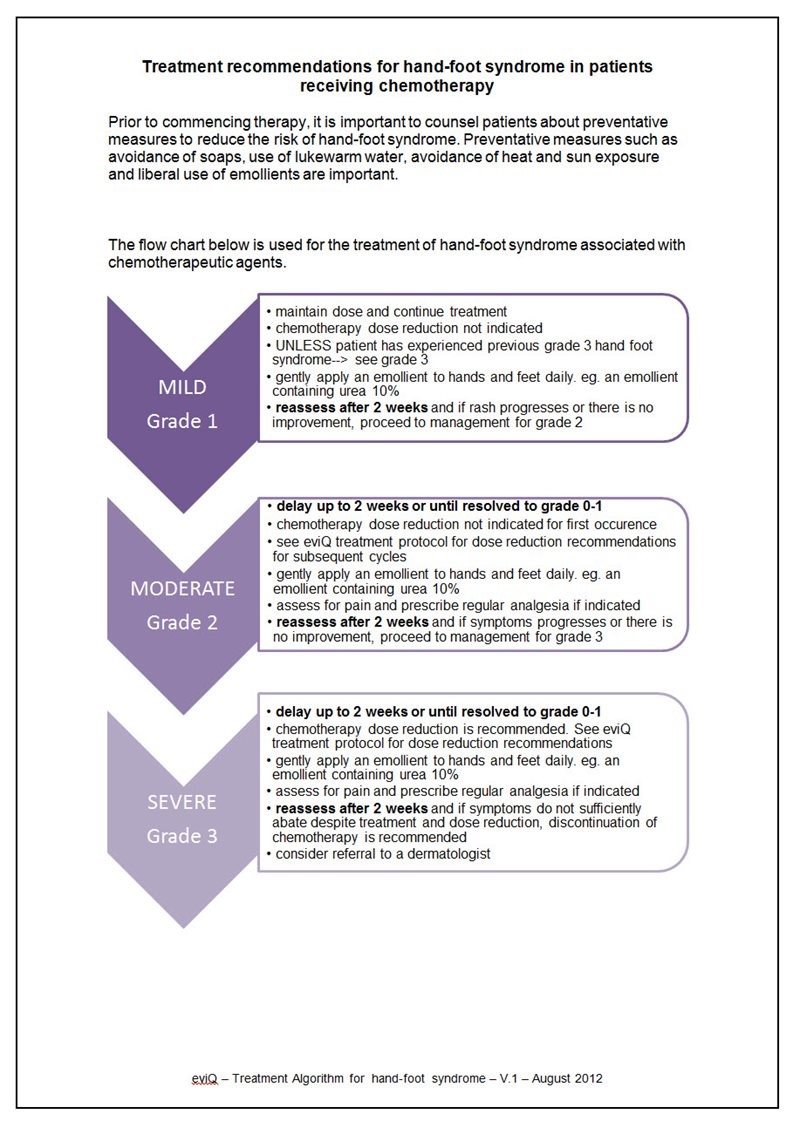
Treatment algorithm:
The treatment algorithm in Figure 1 has been developed by eviQ for the treatment of hand-foot syndrome in patients receiving chemotherapy.
Figure 1. Treatment algorithm for hand-foot syndrome (reproduced with permission from eviQ)
The prognosis for hand-foot syndrome is usually good since the skin condition generally resolves a few weeks after stopping treatment with the responsible drug. However, the condition may recur on restarting treatment.
References:
- Australian Medicines Handbook. AMH [Online]. Adelaide: AMH; 2019.
- NSW Government. Hand-foot syndrome (HFS) – palmar-plantar erythrodysaesthesia (PPE) associated with chemotherapeutic agents. eviQ: Sydney; 2019.
Subscribe Knowledge Centre Updates
Enter your details to receive Knowledge Centre updates
