Yonsa Mpred™ is now listed on the Pharmaceutical Benefits Scheme (PBS) for the treatment of castration-resistant metastatic prostate cancer. Yonsa Mpred™ is supplied as a composite pack containing abiraterone acetate 125mg tablets and methylprednisolone 4mg tablets.
Abiraterone is an inhibitor of cytochrome P450 C17 (CYP17), an enzyme involved in the synthesis of testosterone and other androgens. Studies demonstrate that blocking this enzyme can produce tumour responses in patients who no longer respond to standard hormonal therapies.
Abiraterone also reduces cortisol levels, which leads to a compensatory increase in adrenocorticotropic hormone (ACTH) release. This can result in increased production of adrenal mineralocorticoids, with adverse effects such as hypertension, oedema, and hypokalaemia. The addition of the glucocorticoid, methylprednisolone, suppresses ACTH drive and reduces the incidence and severity of mineralocorticoid excess.
This is the second abiraterone preparation available on the PBS. Zytiga® (abiraterone acetate) tablets exhibit large variations in absorption depending on the fat content of meals. Therefore, these tablets must be taken on an empty stomach. In comparison, the abiraterone in Yonsa Mpred™ was developed to have a smaller particle size, improving bioavailability and allowing tablets to be taken without regard to food. The dosing of these two products is also different. A small study demonstrated therapeutic equivalence between 500mg of fine particle abiraterone acetate (i.e. Yonsa Mpred™) and 1000mg of originator abiraterone acetate based on testosterone suppression.


The Australian Technical Advisory Group on Immunisation (ATAGI) has published advice on seasonal influenza vaccines for 2023. Annual vaccination is recommended for all people six months of age and over and is particularly important for those most at risk.
The National Immunisation Program (NIP) provides free influenza vaccines to the following high-risk groups:
- Children aged six months to less than five years;
- All Aboriginal and Torres Strait Islander people aged six months and over;
- People aged six months and over with certain medical conditions that increase their chance of severe influenza and complications (e.g. certain cardiac, respiratory, neurological, immunocompromising, metabolic, renal, and haematological conditions; and children aged 5-10 years who are taking long-term aspirin therapy);
- Pregnant women (at any stage during pregnancy); and
- People aged 65 years and over.
Table 1 shows the influenza vaccines registered for use in 2023 by age group.
Table 1. 2023 influenza vaccines by age group
| Age group |
Registered influenza vaccines |
| From six months |
Vaxigrip® Tetra |
| Fluarix® Tetra |
| FluQuadri® |
| Influvac® Tetra |
| ≥ 2 years |
Flucelvax® Quad |
| ≥ 5 years |
Afluria® Quad |
| ≥ 60 years |
Fluzone® HighDose Quad |
| ≥ 65 years |
Fluad® Quad |
People 65 years of age and older are at higher risk of developing severe influenza. However, the effectiveness of influenza vaccines is reduced in this age group. Two higher-immunogenicity influenza vaccines are available and are preferred over standard vaccines in this population. Fluad® Quad contains an adjuvant to increase immunogenicity, and Fluzone® HighDose Quad is a higher dose vaccine, containing 240mcg influenza virus haemagglutinin in 0.7mL (compared to 60mcg in 0.5mL for the standard dose vaccines).
There is a lack of data on the co-administration of Fluad® Quad with the adjuvanted shingles vaccine (Shingrix®). While they may be given on the same day, separating the administration by a few days is preferable. ATAGI advises that influenza vaccines can be administered on the same day as any COVID-19 vaccine.
Protection from an influenza vaccine is expected to last for the entire influenza season. However, optimal protection occurs in the three to four months after vaccination. The peak season throughout most of Australia is June to September.


The Pharmaceutical Benefits Scheme (PBS) listing for ruxolitinib has been expanded. The listing now includes acute or chronic graft-versus-host disease (GvHD) in patients with an inadequate response to corticosteroids.
Ruxolitinib is an inhibitor of the Janus Associated Kinases (JAKs), JAK1 and JAK2. Inhibition of these enzymes disrupts cytokine and growth factor signalling pathways involved in the pathogenesis of GvHD. The REACH 2 and REACH 3 studies investigated the safety and efficacy of ruxolitinib compared to control (investigator’s choice of commonly used therapies) in glucocorticoid-refractory GvHD.
The REACH 2 trial was undertaken in patients with acute GvHD. At day 28, the overall response was 62% in the ruxolitinib group compared to 39% in the control group. The REACH 3 trial was conducted in patients with chronic GvHD. At week 24, the overall response was 49.7% in the ruxolitinib group and 25.6% in the control group.
Ruxolitinib is an oral medication with a usual starting dose of 10mg twice daily in chronic GvHD and 5-10mg twice daily in acute GvHD. The dose may require adjustment according to patient response and toxicity or due to interacting drugs. Ruxolitinib is metabolised by CYP3A4 and CYP2C9; the manufacturer recommends halving the dose when administered with dual moderate inhibitors of these enzymes, such as fluconazole ≤ 200mg daily (higher doses of fluconazole should be avoided).


The Therapeutic Goods Administration (TGA) has issued a Medicines Safety Update on the use of pregabalin during pregnancy. The pregnancy risk category for pregabalin has changed from Category B3 to Category D, and product information documents are being updated to strengthen the advice against prescribing pregabalin during pregnancy.
This update is based on the findings of an observational study investigating the safety of pregabalin in the first trimester of pregnancy. Data were obtained from population-based registries in Denmark, Finland, Norway, and Sweden. The incidence of major congenital malformations, birth outcomes, and selected neurodevelopmental outcomes was evaluated for babies exposed to pregabalin in utero. These outcomes were compared to babies exposed to lamotrigine (chosen as an alternative antiepileptic drug), duloxetine (alternative for neuropathic pain and generalised anxiety disorder), and none of these medicines.
The data showed a higher prevalence of major congenital malformations in babies exposed to pregabalin compared with those not exposed to pregabalin or any other antiepileptic drug (crude percentage 5.9% versus 4.1%). However, the adjusted prevalence ratio in the final meta-analysis was not statistically significant (1.13 [95% CI 0.97-1.31]).
The study authors note that their results do not provide strong evidence of human teratogenicity, although a small increased risk cannot be ruled out. The TGA advises that pregabalin should only be prescribed to pregnant women if the benefits clearly outweigh the potential risks.


Several new contraindications have been added to the product information for Paxlovid™ (nirmatrelvir/ritonavir). This medication is now contraindicated with the medications shown in Table 1.
Table 1. New contraindications added to Paxlovid™ product information
| Interacting medicine |
Effect |
Comments |
| Eletriptan |
↑ eletriptan |
Eletriptan is contraindicated within 72 hours of Paxlovid™. Potential for serious adverse effects, including cardiovascular and cerebrovascular events. |
| Silodosin |
↑ silodosin |
Risk of postural hypotension |
| Eplerenone |
↑ eplerenone |
Risk of hyperkalaemia |
| Ivabradine |
↑ ivabradine |
Risk of bradycardia or conduction disturbances |
| Finerenone |
↑ finerenone |
Risk of serious adverse reactions, including hyperkalemia, hypotension, and hyponatremia |
| Naloxegol |
↑ naloxegol |
Potential for opioid withdrawal symptoms |
| Oral midazolam |
↑ midazolam |
Risk of extreme sedation and respiratory
Depression (caution required for parenteral midazolam) |
| Tolvaptan |
↑ tolvaptan |
Risk of dehydration, hypovolemia and hyperkalaemia |
| Primidone |
↓ nirmatrelvir/
ritonavir |
Potential for reduced virologic response and resistance |
| Lumacaftor/Ivacaftor |
↓ nirmatrelvir/
ritonavir |
Potential for reduced virologic response and resistance |
Nirmatrelvir and ritonavir are both substrates of CYP3A, and ritonavir is also a strong inhibitor of this isoenzyme. Concomitant use of medicines that inhibit CYP3A may increase plasma levels of nirmatrelvir/ritonavir, while CYP3A inducers may decrease plasma levels of nirmatrelvir/ritonavir. In addition, nirmatrelvir/ritonavir may increase plasma concentrations of medications metabolised by CYP3A.
The potential consequences of these interactions are:
- Adverse reactions due to increased exposure to concomitant medications;
- Adverse reactions from greater exposure to nirmatrelvir/ritonavir; and
- Reduced therapeutic effect of nirmatrelvir/ritonavir and possible development of viral resistance.
Ritonavir also has a high affinity for P-glycoprotein and several other CYP isoforms and may increase or decrease systemic exposure to many other medicines. Further information on potential drug interactions can be found in the product information or the COVID-19 Drug Interactions website administered by the University of Liverpool, United Kingdom.


The National Immunisation Program (NIP) has updated the vaccination schedule for human papilloma virus (HPV). A single dose of Gardasil® 9 is now recommended for the routine vaccination of young people, with the free catch-up program extended to people under 26 years of age.
This update is supported by the Australian Technical Advisory Group on Immunisation (ATAGI) and the World Health Organization (WHO). Studies, including randomised controlled clinical trials and systematic reviews, indicate that a single dose of HPV vaccine provides similar protection to multidose regimens against initial and persistent infection.
As HPV is responsible for over 95% of cervical cancers, ensuring high vaccination rates is vital. Australia’s vaccination coverage and leading screening and treatment programs have put Australia on track to be the first country to achieve the WHO’s definition of cervical cancer elimination as a public health problem.
Table 1 shows the current HPV vaccine dosing recommendations for different patient populations.
Table 1. Dosing recommendations for HPV vaccines (adapted from Australian Immunisation Handbook)
| Population |
Recommended doses |
Recommended schedule |
| Starting HPV vaccination at 9–25 years of age (except people who are immunocompromised) |
1 |
Single dose |
| Starting HPV vaccination at ≥26 years of age |
3 |
0, 2, 6 months |
| People who are immunocompromised at any age (excluding those with asplenia or hyposplenia) |
3 |
0, 2, 6 months |


Opicapone was added to the Pharmaceutical Benefits Scheme (PBS) on 1 February 2023. Opicapone is indicated as adjunctive therapy to a levodopa-decarboxylase inhibitor combination in adults with Parkinson’s disease who experience end-of-dose motor fluctuations.
Opicapone is an inhibitor of the catechol-O-methyltransferase (COMT) enzyme. When dopa decarboxylase is inhibited (i.e. in patients taking benserazide or carbidopa), COMT becomes a major metabolising enzyme of levodopa. For these patients, opicapone increases levodopa availability in the central nervous system, improving its clinical effect.
A recent meta-analysis compared the safety and efficacy of opicapone (25mg and 50mg orally daily) to placebo in levodopa-treated patients with Parkinson’s disease. Opicapone was associated with reduced time spent in the OFF state and increased time spent in the ON state, including time without troublesome dyskinesia. Patients in the opicapone groups were also more likely to have their levodopa dose reduced. No significant differences were noted between opicapone and placebo regarding serious treatment-emergent adverse events and adverse events leading to study discontinuation.
Entacapone is another COMT inhibitor available in Australia. It requires administration with each levodopa dose, although fixed-dose combination tablets are available with levodopa and carbidopa. In comparison, opicapone has a long duration of action and can be administered once daily. Opicapone capsules should be swallowed whole on an empty stomach at least one hour before or after a levodopa dose.


The product information documents for a number of hydrochlorothiazide-containing products have recently been updated. These products now contain a special warning regarding reports of acute respiratory toxicity.
Acute respiratory toxicity is considered a rare adverse effect associated with hydrochlorothiazide. It presents with pulmonary oedema which can occur within minutes to hours of the initial dose. Early symptoms can include dyspnoea, fever, hypotension, and pulmonary deterioration. Cases can be severe and include acute respiratory distress syndrome (ARDS). Patients who experience ARDS in association with hydrochlorothiazide should not take hydrochlorothiazide again.
Hydrochlorothiazide is a thiazide diuretic indicated for the treatment of hypertension and oedema associated with heart failure, hepatic cirrhosis, or nephrotic syndrome. It is available as a single-ingredient tablet and also in fixed-dose combination with ACE inhibitors, angiotensin II antagonists, or calcium channel blockers. While acute respiratory toxicity is rare, it is important to be aware of due to the relatively common use of hydrochlorothiazide and the potential severity of this adverse effect.
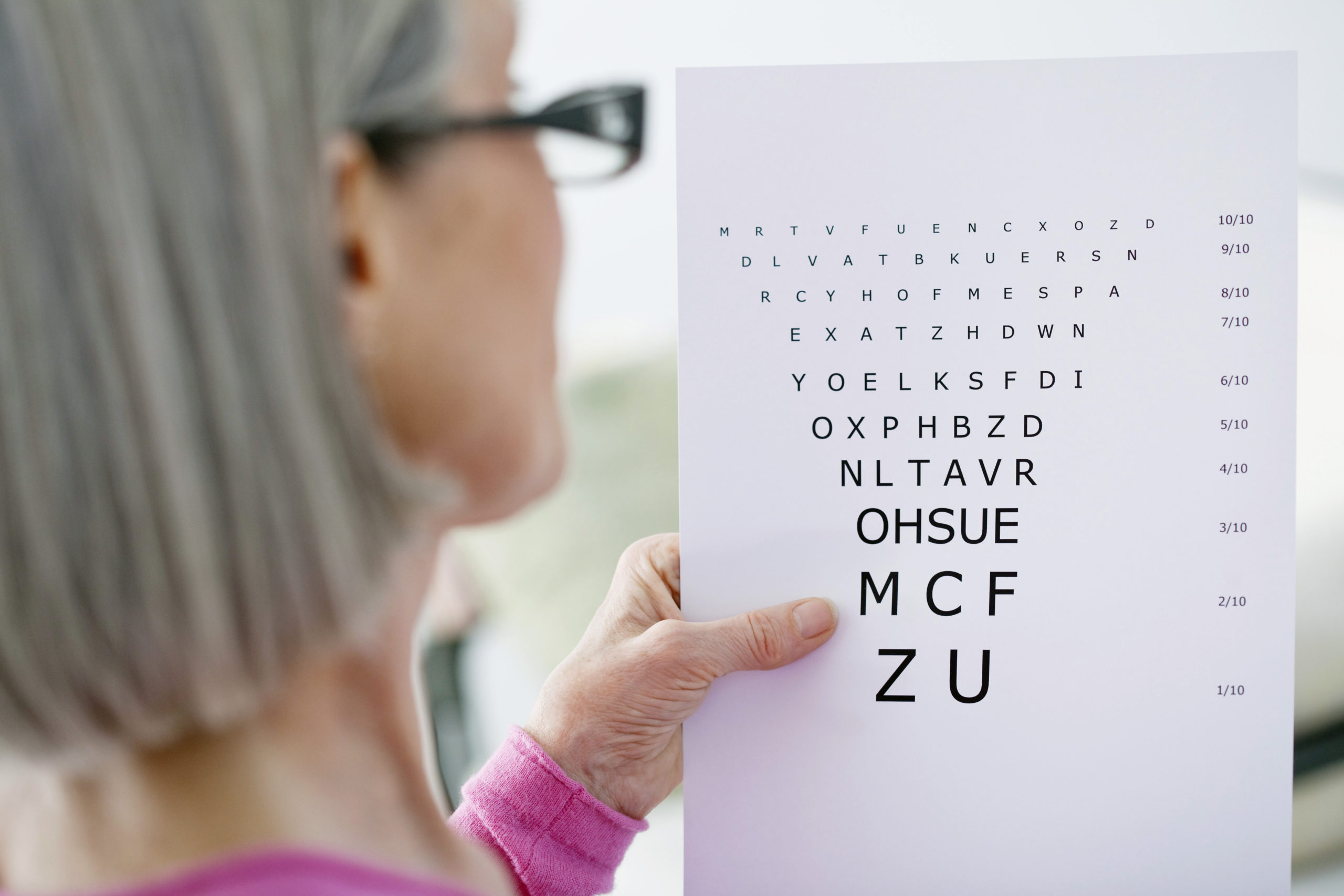
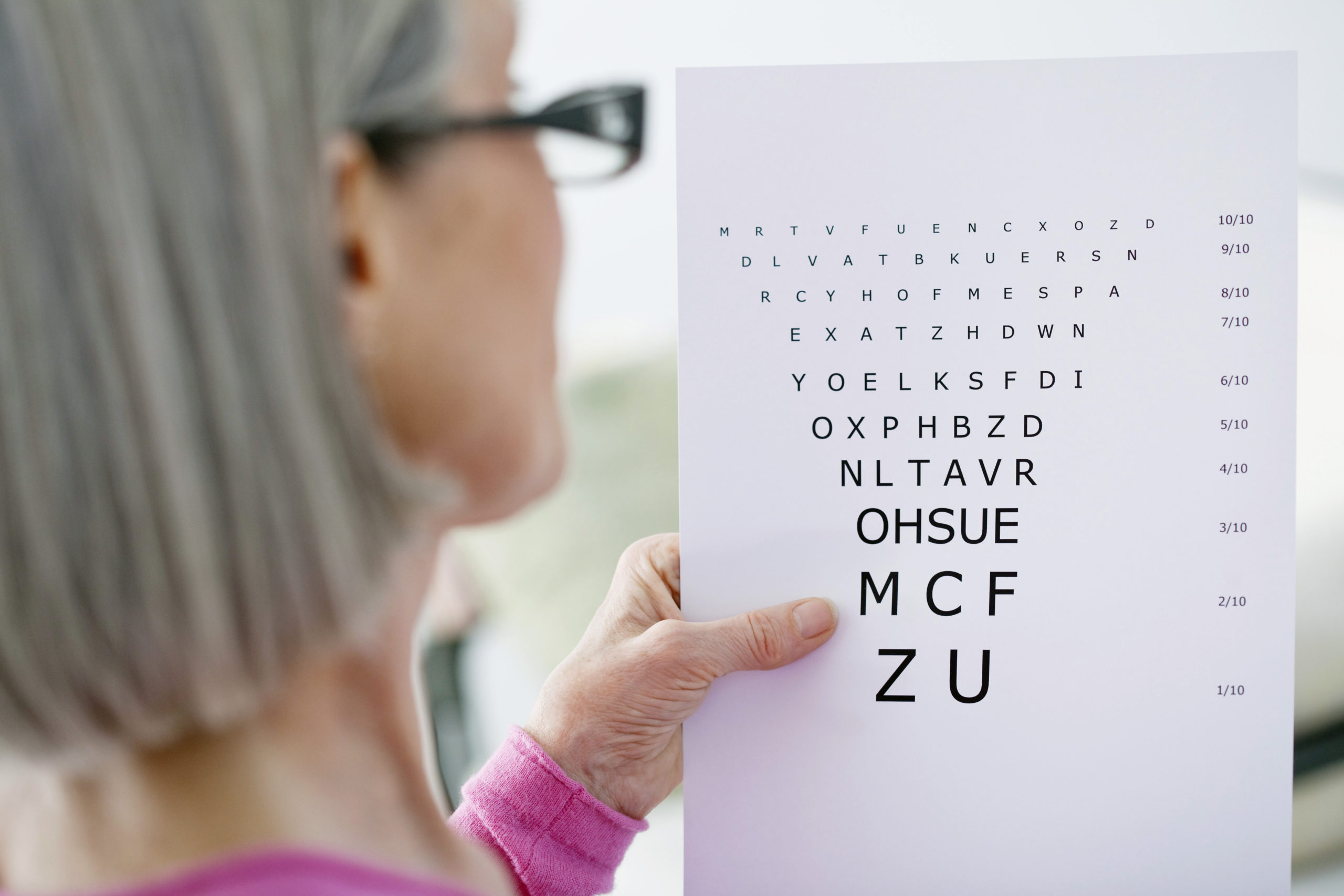
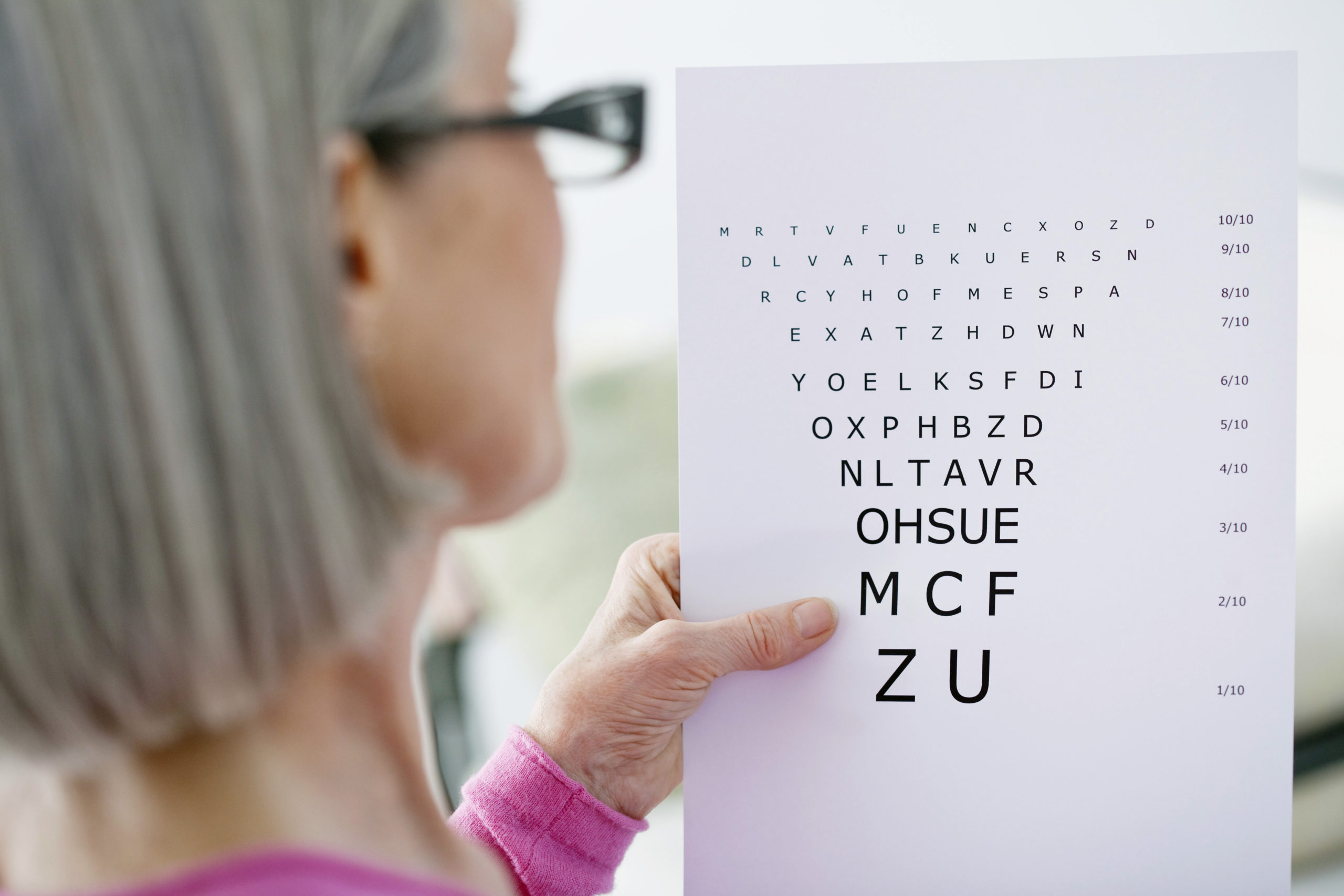
Faricimab has been added to the Pharmaceutical Benefits Scheme (PBS) for the treatment of neovascular (wet) age-related macular degeneration (nAMD) and diabetic macular oedema (DMO).
Faricimab is a monoclonal antibody that inhibits both vascular endothelial growth factor A (VEGF-A) and angiopoietin-2 (Ang2). Inhibition of VEGF-A reduces endothelial cell proliferation, neovascularisation and vascular permeability, while inhibition of Ang2 is thought to increase vascular stability and reduce the effects of VEGF-A on blood vessels. This dual mechanism of action may offer a benefit over medications targeting the VEGF pathway alone, such as aflibercept and ranibizumab.
Another potential benefit of faricimab is the possibility of extending the dosing interval. The manufacturer recommends dosing be initiated at four-weekly intervals for the first four doses. This can then be individualised, with the dosing interval increased up to 16 weeks.
The efficacy of extended dosing intervals was investigated in the TENAYA and LUCERNE trials. Patients with nAMD were randomly assigned to intravitreal faricimab up to every 16 weeks or aflibercept every eight weeks. By week 48, around 45% of faricimab-treated patients were on extended fixed treatment intervals of every 16 weeks, and approximately 80% were on intervals of every 12 weeks or more. The primary endpoint was mean change in best corrected visual acuity (BCVA) from baseline. Faricimab dosing up to every 16 weeks demonstrated non-inferior outcomes compared to aflibercept dosed every eight weeks. Rates of ocular adverse effects were similar for the two treatment groups.
A third medication, pegcetacoplan, was recently added to the Pharmaceutical Benefits Scheme (PBS) to treat paroxysmal nocturnal haemoglobinuria (PNH). This joins the complement C5 inhibitors, eculizumab and ravulizumab, which are also PBS listed for this rare condition.
Pegcetacoplan is indicated for use in patients who have an inadequate response to, or are intolerant of, a complement C5 inhibitor. Inhibitors of C5 reduce haemolysis caused by membrane attack complex (MAC), but haemolysis can still occur due to C3b opsonisation. Studies suggest that polymorphic variations in complement genes may also lead to a poor response to C5 inhibitors in some people. Pegcetacoplan targets upstream sections of the complement cascade (C3 and its activation fragment, C3b) to affect a broader regulation of the complement cascade.
Pegcetacoplan is administered as a twice-weekly subcutaneous infusion. One of the more serious adverse effects is an increased risk of infections. Complement plays a critical role in the immune response to various pathogens, although it appears to be most important against encapsulated bacteria. Therefore, patients receiving pegcetacoplan are at increased risk of infections caused by pathogens such as Streptococcus pneumoniae, Neisseria meningitidis, and Haemophilus influenzae. As these infections can be serious, all patients should be vaccinated against these bacteria at least two weeks before starting pegcetacoplan therapy. If the risk of delaying therapy outweighs the risk of infection, pegcetacoplan may be initiated less than two weeks after vaccination, but patients must receive appropriate prophylactic antibiotics until two weeks after vaccination. The Australian Immunisation Handbook can be referred to for current vaccination advice.